The COVID-19 pandemic resulted in rapid reductions in elective surgery, including surgery as a treatment for head and neck cancer. Healthcare networks produced guidelines and consensus early in the pandemic seeking to provide guidance. Still, with little known about the disease at the time, these were based on opinions, rather than evidence.
The problems were particularly acute in head and neck cancer surgery because, for many cases, a cure is dependent on surgery. However, there was great concern about spreading infection from aerosol-generating procedures in the airway.
Professor Richard Shaw, University of Liverpool and Chair of the Surgery & Localised Therapies Subgroup (NCRI Head & Neck Group)
The role of research networks in gathering rapid evidence: COVIDSurg
The study is part of the COVIDSurg Collaborative, an initiative to describe surgical practices during the early period of the pandemic, when many hospitals had limited capacity and when it was unclear whether it was safer to delay or continue in-hospital cancer treatments.
Members of the NCRI Head and Neck Group acted to provide real-world evidence from during the pandemic to support head and neck surgery practice during the first and forthcoming waves of the pandemic.
Group members utilised the network of research-active clinicians fostered by the NCRI Group structure and the robust UK trial networks as well as engaging researchers abroad through groups such as the European Organisation for Research and Treatment of Cancer (EORTC). The COVID-19 pandemic had a considerable impact on the existing clinical trials activity that the group have developed over the previous years; however, they were able to pivot their activities to support this work in a concise time window.
Evidencing the safety of head and neck cancer surgery
The COVIDSurg study shows head and neck surgery is safe for patients during the COVID-19 pandemic even when lengthy and complex. The results are published in the journal Cancer.
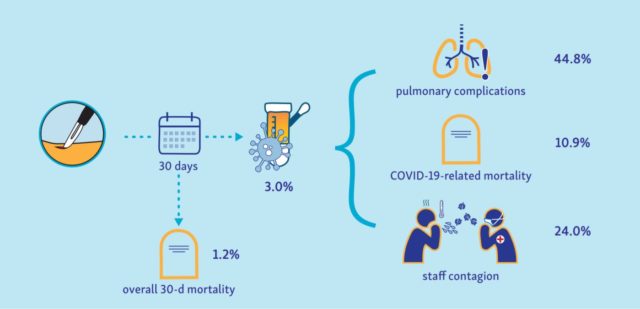
Of over 1000 patients who underwent head and neck cancer surgery during the first wave of the COVID-19 pandemic, the overall 30-day mortality rate was 1.2%, and severe complications of COVID-19 were seen in 1.0%. There was evidence that clinicians moved away from recommending surgery in favour of radiotherapy treatment, and of de-escalation in those receiving surgery, which may not be justified given this reassuring patient safety profile.
The early consensus had been that head and neck surgery was very risky for patients, particularly less fit or elderly patients, or those who required complex procedures or reconstructive surgery. Our data are reassuring in this regard, showing that there is no additional risk of COVID-19 for these groups.
Professor Richard Shaw, University of Liverpool and Chair of the Surgery & Localised Therapies Subgroup (NCRI Head & Neck Group)
A change to current guidance
These results are significant, as concerns over patient safety raised in many guidelines appear not to have been reflected by these outcomes, even for patients with other serious illnesses or who require complex surgery. Researchers recommend that patients who received non-standard treatments should be carefully monitored to optimise their cancer outcomes.
The overlap between patients and surgeons testing positive for the SARS-CoV-2 virus is notable and emphasises the need for thorough infection controls and the use of personal protective equipment.
Implications of treatment delays or changes
Research is ongoing to analyse data from a further 5000 head and neck cancer patients presenting between March and June 2020. The researchers have also received funding to explore the long-term implications of treatment delays or changes for these patients.